After surgery, your body isn’t just healing-it’s rebuilding. Scar tissue forms, muscles tighten, circulation slows, and swelling lingers. You might feel stiff, tired, or frustrated that progress feels slow. What if something as simple as a gentle body massage could help speed things up? It’s not magic. It’s science. And it’s being used in hospitals and rehab centers across the UK-and Brighton, too.
Key Takeaways
- Body massage improves circulation, reduces swelling, and breaks down scar tissue after surgery.
- Lymphatic drainage massage is especially effective for reducing fluid buildup in the first 2-6 weeks post-op.
- Massage should start only after your surgeon gives clearance-usually 1-3 weeks after surgery, depending on the procedure.
- Avoid deep pressure near incisions; light, rhythmic strokes are safest and most effective.
- Combining massage with gentle movement (like walking) boosts recovery faster than either alone.
Why Body Massage Matters After Surgery
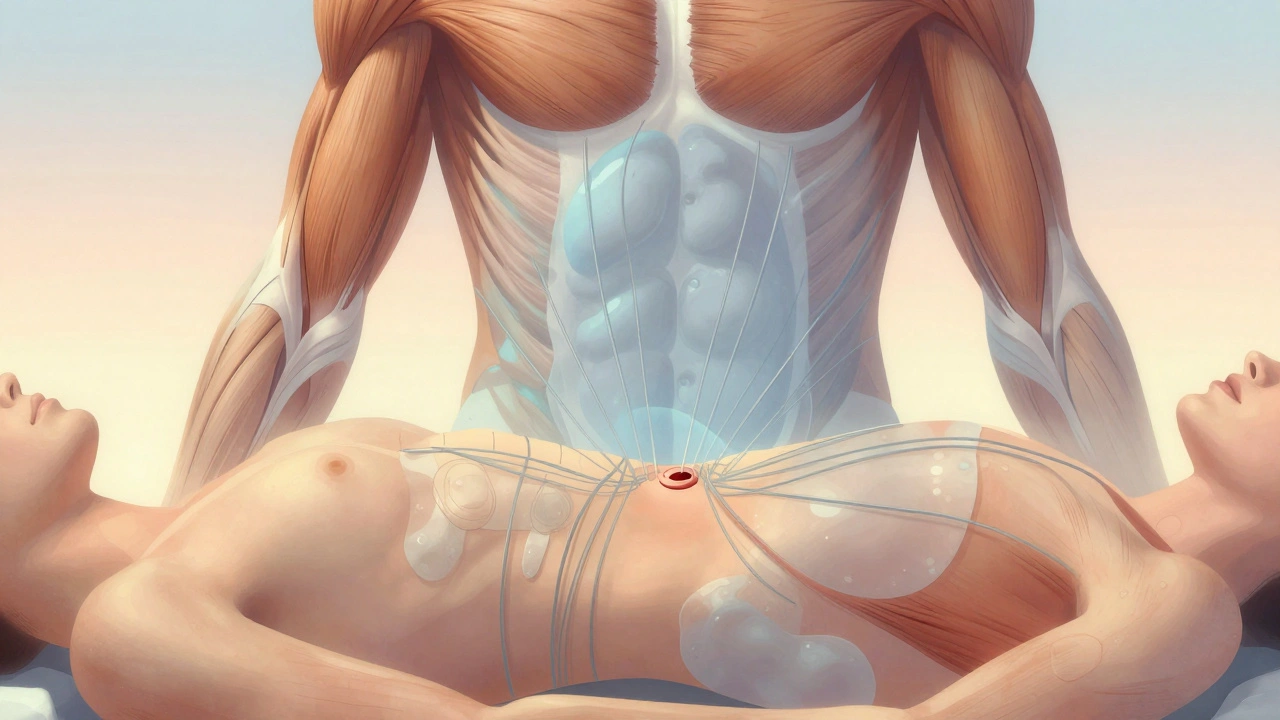
Think of your body after surgery like a construction site. The surgeon fixed the main structure, but now the cleanup crew needs to come in: removing debris, restoring flow, and calming the chaos. That’s where massage steps in.
When you undergo surgery, your body goes into survival mode. Blood flow slows around the surgical area. Fluid pools. Muscles tense up as a protective reflex. Scar tissue starts forming within days-sometimes becoming stiff, painful, or restrictive.
Studies from the Journal of Clinical Nursing show that patients who received gentle manual therapy within the first two weeks after abdominal or orthopedic surgery reported 30% less pain and 25% faster mobility compared to those who didn’t. It’s not about relaxation-it’s about function.
You don’t need to wait until you’re ‘fully healed’ to start. In fact, waiting too long can make recovery harder. The goal isn’t to fix everything at once. It’s to gently guide your body back to normal movement and circulation.
What Types of Massage Help After Surgery?
Not all massages are created equal when you’re recovering. You need something precise-not a full-body indulgence.
- Lymphatic Drainage Massage (LDM): This is the gold standard for post-surgery recovery. It uses feather-light pressure to move excess fluid away from swollen areas. Think of it like opening tiny drains in your tissues. It’s especially helpful after breast surgery, liposuction, or joint replacements.
- Swedish Massage (Light Version): Gentle strokes, slow kneading, and circular motions help relax surrounding muscles without disturbing healing tissue. Ideal for patients recovering from spine or hip surgery.
- Myofascial Release: Targets tight bands of connective tissue (fascia) that form after trauma. Used carefully, it can improve range of motion without reopening incisions.
What’s NOT safe? Deep tissue, trigger point therapy, or anything with intense pressure near the surgical site. Even sports massage-often great for athletes-is too aggressive right after surgery.
When Can You Start Massage After Surgery?
This isn’t a one-size-fits-all answer. Timing depends on the surgery, your health, and your surgeon’s protocol.
- Minor procedures (like laparoscopic gallbladder removal): You may start gentle LDM after 7-10 days.
- Major orthopedic surgery (knee or hip replacement): Most surgeons recommend waiting 2-3 weeks, then starting with 10-15 minute sessions 2-3 times a week.
- Cancer-related surgeries (mastectomy, lymph node removal): Lymphatic drainage often begins within 10-14 days, but only under supervision of a trained therapist.
Always get written clearance from your surgeon or physiotherapist before starting. If you have drains, stitches, or open wounds, massage is off-limits until they’re fully healed.
What Happens During a Post-Surgery Massage Session?
It’s nothing like a spa day. There’s no music, no candles, no oils-just quiet focus.
You’ll lie on a padded table, covered with a sheet. The therapist will ask you where you feel tightness, numbness, or swelling. They’ll avoid your incision entirely, working around it with slow, rhythmic movements.
A typical session lasts 30-45 minutes. You might feel a slight tingling as fluid moves, or a warm sensation as blood flow returns. Some people feel a bit tired afterward-this is normal. Your body is working hard to rebalance itself.
Most therapists use a technique called manual lymphatic drainage: light, circular motions, like brushing your skin with a feather. No digging. No kneading. Just gentle redirection of fluid.
Where to Find Post-Surgery Massage Services in Brighton
Brighton has several clinics specializing in medical massage therapy. Look for therapists with certifications in Lymphatic Drainage Therapy or Manual Lymphatic Drainage (MLD) from recognized bodies like the Lymphoedema Support Network or the British Association of Massage Therapists.
- Brighton Medical Massage Clinic (Kemptown): Offers post-op LDM with physiotherapists on staff. Accepts referrals from NHS consultants.
- The Healing Room (North Laine): Specializes in cancer recovery massage. Trained in post-mastectomy care.
- Wellbeing Physio & Massage (Hove): Works with orthopedic surgeons to create personalized recovery plans.
Ask if they’ve worked with patients after your type of surgery. A good therapist will ask you about your procedure, medications, and pain levels before even touching you.
Cost and Booking
Most post-surgery massage sessions in Brighton cost between £50 and £75 for a 45-minute treatment. Some clinics offer package deals-three sessions for £180, for example.
Insurance doesn’t always cover it, but if you’re recovering through NHS physio, ask if they can refer you to a certified therapist. Some NHS trusts have partnerships with local clinics for post-op care.
Book ahead. These therapists often have waiting lists, especially after holiday seasons when surgeries spike.

Safety Tips: What to Avoid
Recovery is fragile. A wrong move can delay healing-or cause harm.
- Don’t massage directly over incisions-even if they look healed. Underneath, tissue is still repairing.
- Avoid heat packs or hot stones near surgical areas. Heat increases swelling.
- Stop immediately if you feel sharp pain, numbness, or increased swelling.
- Don’t combine massage with blood thinners without checking with your doctor. Some medications increase bruising risk.
- Stay hydrated. Massage moves fluid-your kidneys need water to flush it out.
Body Massage vs. Physiotherapy After Surgery
| Aspect | Body Massage | Physiotherapy |
|---|---|---|
| Primary Goal | Reduce swelling, improve circulation, relax surrounding tissue | Restore movement, rebuild strength, correct posture |
| Pressure Used | Very light to moderate | Varies-can include stretching, resistance, joint mobilization |
| When to Start | Usually 1-3 weeks post-op | Often starts within days, even with drains or braces |
| Best For | Fluid buildup, tightness, pain relief | Mobility loss, muscle weakness, balance issues |
| Who Delivers It | Massage therapist with MLD certification | Chartered physiotherapist |
| Insurance Coverage | Usually not covered | Often covered by private health insurance |
They’re not rivals-they’re teammates. Many patients do both: massage to calm the area, then physio to rebuild function. One softens the tissue; the other reteaches the body how to move.
Frequently Asked Questions
Can massage help with scar tissue after surgery?
Yes-gently. After 4-6 weeks, once the incision is fully closed, light myofascial release or cross-friction massage can help break up dense scar tissue. This improves flexibility and reduces pulling sensations. Never rub aggressively-use just enough pressure to feel a slight tug, not pain. Many patients report less tightness and better movement after 3-5 sessions.
Is it safe to get a massage after having a stent or pacemaker?
Generally yes, but avoid direct pressure over the device site. For example, if you had a pacemaker implanted under your left collarbone, the therapist should work around that area, not on it. Always inform your therapist about any implants. Most are designed to withstand normal daily pressure-massage won’t damage them, but it’s better to be cautious.
How many massage sessions do I need after surgery?
It varies. For minor surgeries, 2-4 sessions over 3-4 weeks often makes a noticeable difference. For major procedures like hip replacement or cancer surgery, 6-10 sessions spread over 8-12 weeks is common. Think of it like physical rehab-you wouldn’t expect one gym session to fix a year of inactivity. Consistency matters more than intensity.
Can I do self-massage after surgery?
Yes-but only in areas away from the incision. For example, if you had knee surgery, you can gently stroke your calf or thigh (not the knee itself) with light, upward motions toward your heart. Use lotion or oil to reduce friction. Never press hard or use tools like foam rollers near the surgical site. Your therapist can show you simple techniques to do at home between sessions.
Will massage make me bruise more after surgery?
If done correctly, no. Lymphatic drainage uses pressure so light it’s like brushing a fly off your skin. Deep pressure can cause bruising, but that’s not what’s used in post-surgery care. If you notice unusual bruising, swelling, or warmth after a session, stop and contact your doctor. It could be a sign of a blood clot or infection.
Ready to Move Better?
Recovery doesn’t have to feel like a slow crawl. Massage isn’t a luxury-it’s a tool. A quiet, powerful one that helps your body do what it’s already trying to do: heal. If you’re still stiff, swollen, or sore weeks after surgery, don’t just wait it out. Talk to your care team. Ask if massage therapy is right for you. In Brighton, trained therapists are waiting to help you move again-without pain, without fear, without delay.









Melissa Pemberton
January 9, 2026 AT 02:02Hannah Ronquillo
January 10, 2026 AT 18:32Tim Paradis
January 11, 2026 AT 05:53Ken Chess
January 11, 2026 AT 07:42Darshan R
January 12, 2026 AT 00:11alyssa golightly
January 13, 2026 AT 19:07Vicky Durel
January 14, 2026 AT 01:35Mrigank Srivastava
January 15, 2026 AT 13:44Kristina Mozdzierz
January 16, 2026 AT 12:14